Search
- Page Path
- HOME > Search
- Miscellaneous
- AM1638, a GPR40-Full Agonist, Inhibited Palmitate- Induced ROS Production and Endoplasmic Reticulum Stress, Enhancing HUVEC Viability in an NRF2-Dependent Manner
- Hwan-Jin Hwang, Joo Won Kim, SukHwan Yun, Min Jeong Park, Eyun Song, Sooyeon Jang, Ahreum Jang, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
- Endocrinol Metab. 2023;38(6):760-769. Published online November 2, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1774

- 1,206 View
- 85 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
G protein-coupled receptor 40 (GPR40) is a key molecule in diabetes and fatty liver, but its role in endothelial dysfunction remains unclear. Our objective in this study was to determine whether GPR40 agonists protect endothelial cells against palmitatemediated oxidative stress.
Methods
Human umbilical vein endothelial cells (HUVECs) were used to investigate effects of various GPR40 agonists on vascular endothelium.
Results
In HUVECs, AM1638, a GPR40-full agonist, enhanced nuclear factor erythroid 2–related factor 2 (NRF2) translocation to the nucleus and heme oxygenase-1 (HO-1) expression, which blocked palmitate-induced superoxide production. Those antioxidant effects were not detected after treatment with LY2922470 or TAK875, GPR40-partial agonists, suggesting that GPR40 regulates reactive oxygen species (ROS) removal in a ligand-dependent manner. We also found that palmitate-induced CCAAT/enhancer‐binding protein homologous protein expression; X-box binding protein-1 splicing, nuclear condensation, and fragmentation; and caspase-3 cleavage were all blocked in an NRF2-dependent manner after AM1638 treatment. Both LY2922470 and TAK875 also improved cell viability independent of the NRF2/ROS pathway by reducing palmitate-mediated endoplasmic reticulum stress and nuclear damage. GPR40 agonists thus have beneficial effects against palmitate in HUVECs. In particular, AM1638 reduced palmitate-induced superoxide production and cytotoxicity in an NRF2/HO-1 dependent manner.
Conclusion
GPR40 could be developed as a good therapeutic target to prevent or treat cardiovascular diseases such as atherosclerosis.

- Diabetes, Obesity and Metabolism
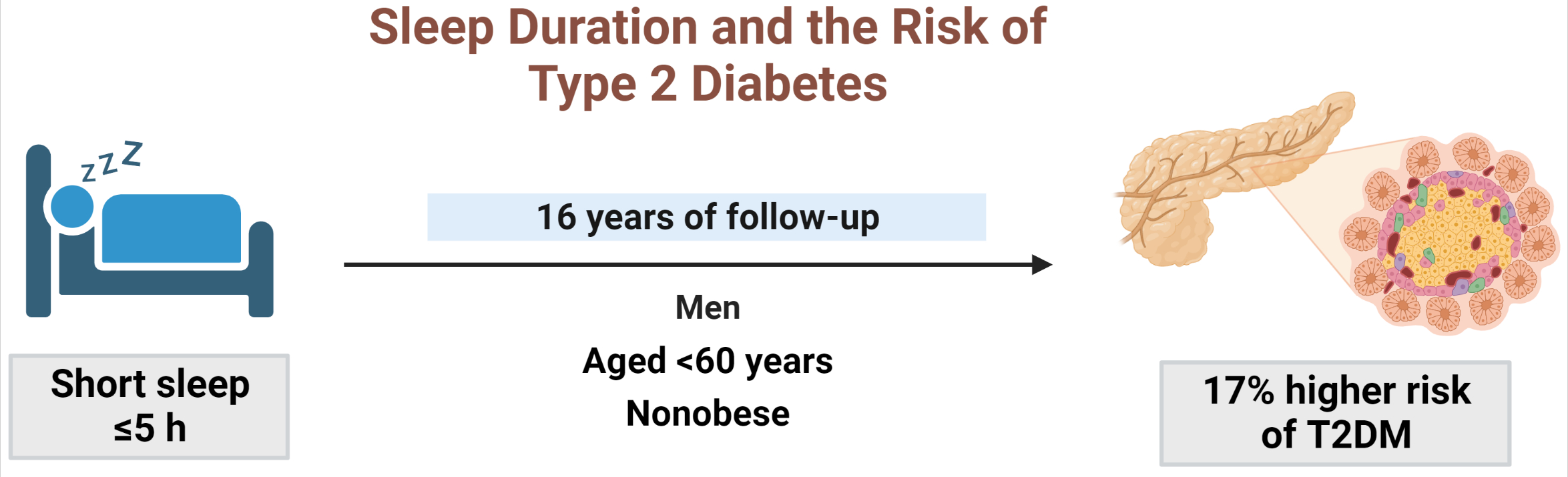
- Sleep Duration and the Risk of Type 2 Diabetes: A Community-Based Cohort Study with a 16-Year Follow-up
- Da Young Lee, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Seung Ku Lee, Chol Shin, Nan Hee Kim
- Endocrinol Metab. 2023;38(1):146-155. Published online February 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1582
- 2,632 View
- 165 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
We aimed to investigate the moderating effects of obesity, age, and sex on the association between sleep duration and the development of diabetes in Asians.
Methods
We analyzed data from a cohort of the Korean Genome and Epidemiology Study conducted from 2001 to 2020. After excluding shift workers and those with diabetes at baseline, 7,407 participants were stratified into three groups according to sleep duration: ≤5 hours/night, >5 to 7 hours/night (reference), and >7 hours/night. The Cox proportional hazards analyses were used to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) for incident type 2 diabetes mellitus (T2DM). Subgroup analyses were performed according to obesity, age, and sex.
Results
During 16 years of follow-up, 2,024 cases of T2DM were identified. Individuals who slept ≤5 h/night had a higher risk of incident diabetes than the reference group (HR, 1.17; 95% CI, 1.02 to 1.33). The subgroup analysis observed a valid interaction with sleep duration only for obesity. A higher risk of T2DM was observed in the ≤5 hours/night group in non-obese individuals, men, and those aged <60 years, and in the >7 hours/night group in obese individuals (HRs were 1.34 [95% CI, 1.11 to 1.61], 1.22 [95% CI, 1 to 1.49], and 1.18 [95% CI, 1.01 to 1.39], respectively).
Conclusion
This study confirmed the effect of sleep deprivation on the risk of T2DM throughout the 16-year follow-up period. This impact was confined to non-obese or young individuals and men. We observed a significant interaction between sleep duration and obesity. -
Citations
Citations to this article as recorded by- Attention to Innate Circadian Rhythm and the Impact of Its Disruption on Diabetes
Da Young Lee, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Nan Hee Kim
Diabetes & Metabolism Journal.2024; 48(1): 37. CrossRef - Role of Sleep and Sleep Disorders in Cardiometabolic Risk: a Review and Update
Shaden O. Qasrawi, Ahmed S. BaHammam
Current Sleep Medicine Reports.2024; 10(1): 34. CrossRef - Evaluating reliability in wearable devices for sleep staging
Vera Birrer, Mohamed Elgendi, Olivier Lambercy, Carlo Menon
npj Digital Medicine.2024;[Epub] CrossRef - All That Glitters Is Not Gold: The Same Sleep Time, but Different Diabetogenic Outcomes
Bohye Kim, Obin Kwon
Endocrinology and Metabolism.2023; 38(1): 78. CrossRef - The Link Between Sleeping and Type 2 Diabetes: A Systematic Review
Ali Darraj
Cureus.2023;[Epub] CrossRef
- Attention to Innate Circadian Rhythm and the Impact of Its Disruption on Diabetes

- Diabetes, Obesity and Metabolism
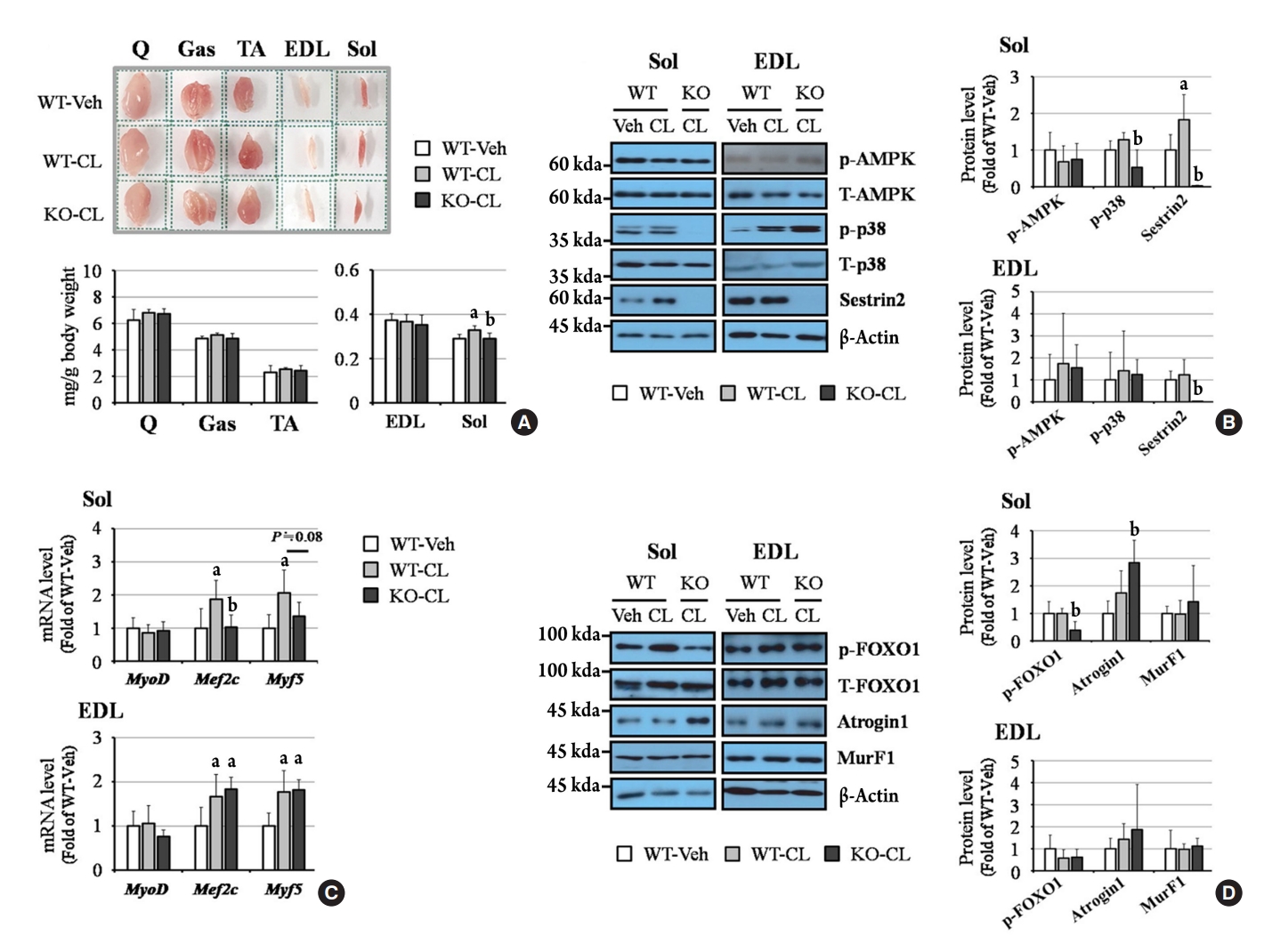
- Sestrin2 Regulates Beneficial β3-Adrenergic Receptor-Mediated Effects Observed in Inguinal White Adipose Tissue and Soleus Muscle
- Min Jeong Park, Joo Won Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Hwan-Jin Hwang, Hye Jin Yoo
- Endocrinol Metab. 2022;37(3):552-557. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1421
- 2,640 View
- 107 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Sestrin2, a well-known adenosine monophosphate-activated protein kinase (AMPK) regulator, plays a protective role against metabolic stress. The β3-adrenergic receptor (β3AR) induces fat browning and inhibits muscle atrophy in an AMPK-dependent manner. However, no prior research has examined the relationship of sestrin2 with β3AR in body composition changes. In this study, CL 316,243 (CL), a β3AR agonist, was administered to wild-type and sestrin2-knockout (KO) mice for 2 weeks, and fat and muscle tissues were harvested. CL induced AMPK phosphorylation, expression of brown-fat markers, and mitochondrial biogenesis, which resulted in the reduction of lipid droplet size in inguinal white adipose tissue (iWAT). These effects were not observed in sestrin2-KO mice. In CL-treated soleus muscle, sestrin2-KO was related to decreased myogenic gene expression and increased levels of muscle atrophy-related molecules. Our results suggest that sestrin2 is associated with beneficial β3AR-mediated changes in body composition, especially in iWAT and in the soleus.
-
Citations
Citations to this article as recorded by- Sestrin2 levels in patients with anxiety and depression myocardial infarction was up-regulated and suppressed inflammation and ferroptosis by LKB1-mediated AMPK activation
Yufeng Qian, Lian Chen, Beibei Gao, Xianhua Ye
Clinical and Experimental Hypertension.2023;[Epub] CrossRef - Sestrin2 in diabetes and diabetic complications
Xiaodan Zhang, Zirui Luo, Jiahong Li, Yaxuan Lin, Yu Li, Wangen Li
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Sestrin2 levels in patients with anxiety and depression myocardial infarction was up-regulated and suppressed inflammation and ferroptosis by LKB1-mediated AMPK activation

- Thyroid
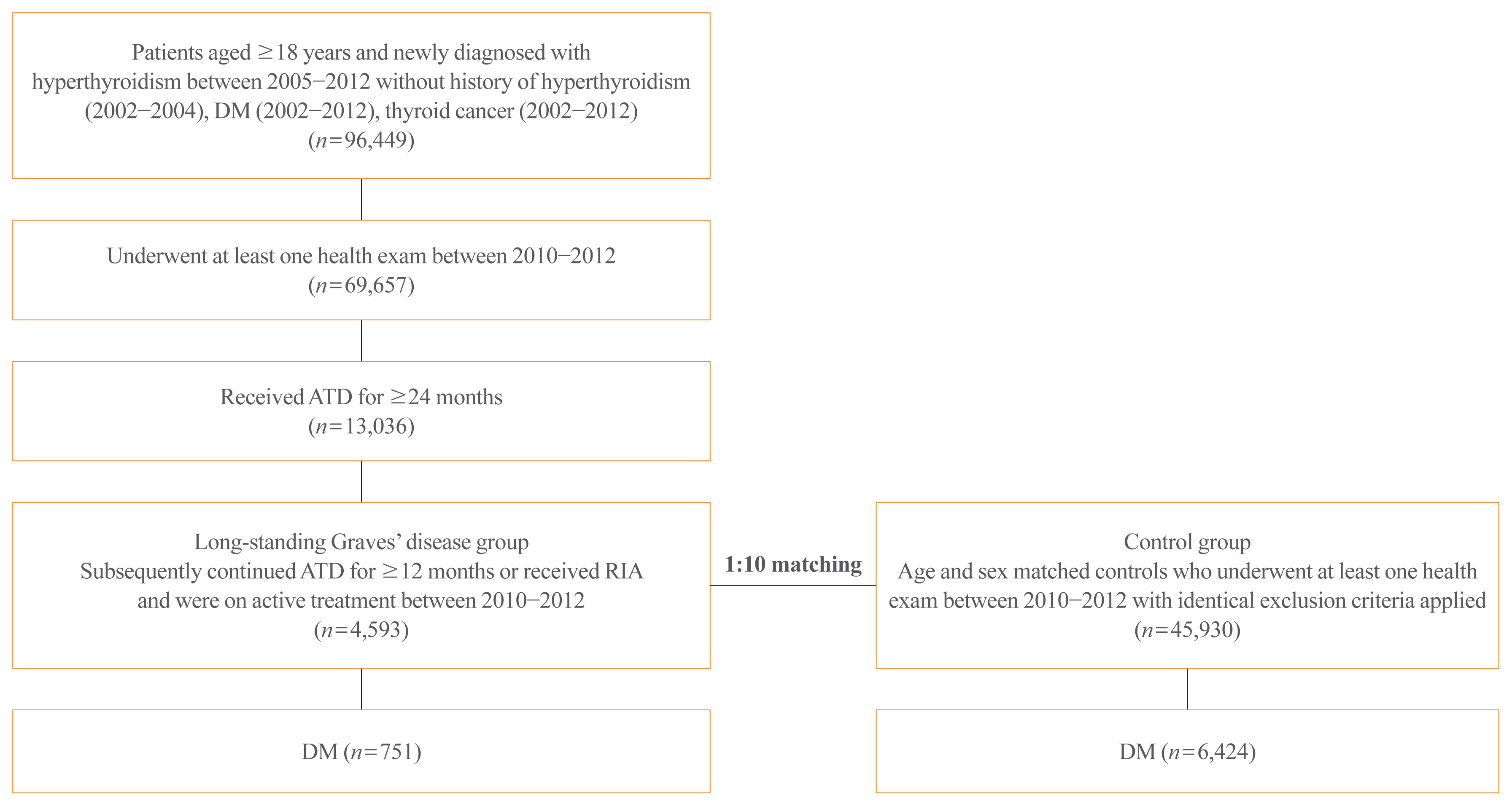
Big Data Articles (National Health Insurance Service Database) - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
- Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
- Endocrinol Metab. 2021;36(6):1277-1286. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1251
- 5,188 View
- 181 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The detrimental effects of excessive thyroid hormone on glucose metabolism have been widely investigated. However, the risk of diabetes in patients with long-standing hyperthyroidism, especially according to treatment modality, remains uncertain, with few longitudinal studies.
Methods
The risk of diabetes in patients with Graves’ disease treated with antithyroid drugs (ATDs) for longer than the conventional duration (≥2 years) was compared with that in age-and sex-matched controls. The risk was further compared according to subsequent treatment modalities after a 24-month course of ATD: continuation of ATD (ATD group) vs. radioactive iodine ablation (RIA) group.
Results
A total of 4,593 patients were included. Diabetes was diagnosed in 751 (16.3%) patients over a follow-up of 7.3 years. The hazard ratio (HR) for diabetes, after adjusting for various known risk factors, was 1.18 (95% confidence interval [CI], 1.10 to 1.28) in patients with hyperthyroidism. Among the treatment modality groups, the RIA group (n=102) had a higher risk of diabetes than the ATD group (n=4,491) with HR of 1.56 (95% CI, 1.01 to 2.42). Further, the risk of diabetes increased with an increase in the ATD treatment duration (P for trend=0.019).
Conclusion
The risk of diabetes was significantly higher in patients with long-standing Graves’ disease than in the general population, especially in patients who underwent RIA and prolonged ATD treatment. Special attention to hyperglycemia during follow-up along with effective control of hyperthyroidism may be necessary to reduce the risk of diabetes in these patients. -
Citations
Citations to this article as recorded by- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience
Nadia Sawicka-Gutaj, Dawid Gruszczyński, Natalia Zawalna, Kacper Nijakowski, Agnieszka Skiba, Mateusz Pochylski, Jerzy Sowiński, Marek Ruchała
Pharmacological Reports.2024; 76(1): 185. CrossRef - Increased risk of diabetes mellitus and hyperlipidemia in patients with differentiated thyroid cancer
Hwa Young Ahn, Jooyoung Lee, Jinmo Kang, Eun Kyung Lee
European Journal of Endocrinology.2024; 190(3): 248. CrossRef - Prevalencia de diabetes en personas con disfunción tiroidea
Juan J. Díez, Pedro Iglesias
Medicina Clínica.2023; 160(8): 333. CrossRef - Control of Thyroid Dysfunction in Spanish Population Registered in
the Primary Care Clinical Database: An Analysis of the Proportion of Patients
with Thyrotropin Values Outside the Reference Range
Juan J. Díez, Pedro Iglesias
Hormone and Metabolic Research.2023; 55(03): 184. CrossRef - Prevalence of thyroid dysfunction and its relationship to income level and employment status: a nationwide population-based study in Spain
Juan J. Díez, Pedro Iglesias
Hormones.2023; 22(2): 243. CrossRef - Prevalence of diabetes in people with thyroid dysfunction
Juan J. Díez, Pedro Iglesias
Medicina Clínica (English Edition).2023; 160(8): 333. CrossRef - Diabetes Mellitus Secondary to Endocrine Diseases: An Update of Diagnostic and Treatment Particularities
Mihaela Simona Popoviciu, Lorena Paduraru, Raluca Marinela Nutas, Alexandra Maria Ujoc, Galal Yahya, Kamel Metwally, Simona Cavalu
International Journal of Molecular Sciences.2023; 24(16): 12676. CrossRef - Thyroid Eye Disease and Its Association With Diabetes Mellitus: A Major Review
Roshmi Gupta, Pramila Kalra, Lakshmi B. Ramamurthy, Suryasnata Rath
Ophthalmic Plastic & Reconstructive Surgery.2023; 39(6S): S51. CrossRef - Metabolite Changes during the Transition from Hyperthyroidism to Euthyroidism in Patients with Graves’ Disease
Ho Yeop Lee, Byeong Chang Sim, Ha Thi Nga, Ji Sun Moon, Jingwen Tian, Nguyen Thi Linh, Sang Hyeon Ju, Dong Wook Choi, Daiki Setoyama, Hyon-Seung Yi
Endocrinology and Metabolism.2022; 37(6): 891. CrossRef - Diabetes and Hyperthyroidism: Is There a Causal Link?
Sang Yong Kim
Endocrinology and Metabolism.2021; 36(6): 1175. CrossRef
- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience

- Clinical Study
- Achievement of LDL-C Targets Defined by ESC/EAS (2011) Guidelines in Risk-Stratified Korean Patients with Dyslipidemia Receiving Lipid-Modifying Treatments
- Ye Seul Yang, Seo Young Lee, Jung-Sun Kim, Kyung Mook Choi, Kang Wook Lee, Sang-Chol Lee, Jung Rae Cho, Seung-Jin Oh, Ji-Hyun Kim, Sung Hee Choi
- Endocrinol Metab. 2020;35(2):367-376. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.367

- 8,000 View
- 144 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study assessed the proportion of risk-stratified Korean patients with dyslipidemia achieving their low-density lipoprotein cholesterol (LDL-C) targets as defined by the European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) (2011) guidelines while receiving lipid-modifying treatments (LMTs).
Methods
In this multicenter, cross-sectional, observational study, we evaluated data from Korean patients aged ≥19 years who were receiving LMTs for ≥3 months and had an LDL-C value within the previous 12 months on the same LMT. Data were collected for demographics, cardiovascular (CV) risk factors, medical history, and healthcare consumption. Patients were risk-stratified according to the ESC Systematic COronary Risk Evaluation (SCORE) chart and LDL-C target achievement rate was assessed.
Results
Guideline-based risk-stratification of the 1,034 patients showed the majority (72.2%) to be in the very high-risk category. Investigators’ assessment of risk was underestimated in 71.6% compared to ESC/EAS guidelines. Overall LDL-C target achievement rate was 44.3%; target achievement was the highest (66.0%) in moderate-risk patients and the lowest (39.0%) in very high-risk patients. Overall 97.1% patients were receiving statin therapy, mostly as a single-agent (89.2%). High-intensity statins and the highest permissible dose of high-intensity statins had been prescribed to only 9.1% and 7.3% patients in the very high-risk group, respectively. Physician satisfaction with patients’ LDL-C levels was the primary reason for non-intensification of statin therapy.
Conclusion
Achievement of target LDL-C level is suboptimal in Korean patients with dyslipidemia, especially in those at very high-risk of CV events. Current practices in LMTs need to be improved based on precise CV risk evaluation posed by dyslipidemia. -
Citations
Citations to this article as recorded by- Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Bempedoic Acid for Lipid Management in the Indian Population: An Expert Opinion
Jagdish Hiremath, J C Mohan, Prakash Hazra, JP S Sawhney, Ashwani Mehta, Sadanand Shetty, Abraham Oomman, Mahesh K Shah, Ganapathi Bantwal, Rajeev Agarwal, Rajiv Karnik, Peeyush Jain, Saumitra Ray, Sambit Das, Vibhuti Jadhao, Sachin Suryawanshi, Hanmant B
Cureus.2023;[Epub] CrossRef - Optimal implementation of the 2019 ESC/EAS dyslipidaemia guidelines in patients with and without atherosclerotic cardiovascular disease across Europe: a simulation based on the DA VINCI study
Julia Brandts, Sarah Bray, Guillermo Villa, Alberico L. Catapano, Neil R. Poulter, Antonio J. Vallejo-Vaz, Kausik K. Ray
The Lancet Regional Health - Europe.2023; 31: 100665. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Target Low-Density Lipoprotein-Cholesterol and Secondary Prevention for Patients with Acute Myocardial Infarction: A Korean Nationwide Cohort Study
Ju Hyeon Kim, Jung-Joon Cha, Subin Lim, Jungseok An, Mi-Na Kim, Soon Jun Hong, Hyung Joon Joo, Jae Hyoung Park, Cheol Woong Yu, Do-Sun Lim, Kyeongmin Byeon, Sang-Wook Kim, Eun-Seok Shin, Kwang Soo Cha, Jei Keon Chae, Youngkeun Ahn, Myung Ho Jeong, Tae Hoo
Journal of Clinical Medicine.2022; 11(9): 2650. CrossRef - Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines
Soo Jin Yun, In-Kyung Jeong, Jin-Hye Cha, Juneyoung Lee, Ho Chan Cho, Sung Hee Choi, SungWan Chun, Hyun Jeong Jeon, Ho-Cheol Kang, Sang Soo Kim, Seung-Hyun Ko, Gwanpyo Koh, Su Kyoung Kwon, Jae Hyuk Lee, Min Kyong Moon, Junghyun Noh, Cheol-Young Park, Sung
Diabetes & Metabolism Journal.2022; 46(3): 464. CrossRef - There is urgent need to treat atherosclerotic cardiovascular disease risk earlier, more intensively, and with greater precision: A review of current practice and recommendations for improved effectiveness
Michael E. Makover, Michael D. Shapiro, Peter P. Toth
American Journal of Preventive Cardiology.2022; 12: 100371. CrossRef - Non-achievement of the Low-Density Lipoprotein Cholesterol Goal in Older Patients with Type 2 Diabetes Mellitus and a Very High Cardiovascular Disease Risk: A Multicenter Study in Vietnam
Huan Thanh Nguyen, Khang Pham Trong Ha, An Huu Nguyen, Thu Thanh Nguyen, Hang My Lam
Annals of Geriatric Medicine and Research.2021; 25(4): 278. CrossRef
- Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement

- Clinical Study
- Impact of the Dynamic Change of Metabolic Health Status on the Incident Type 2 Diabetes: A Nationwide Population-Based Cohort Study
- Jung A Kim, Da Hye Kim, Seon Mee Kim, Yong Gyu Park, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi, Kyungdo Han, Hye Jin Yoo
- Endocrinol Metab. 2019;34(4):406-414. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.406
- 5,992 View
- 84 Download
- 16 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Metabolically healthy obese (MHO) is regarded as a transient concept. We examined the effect of the dynamic change of metabolic health status on the incidence of type 2 diabetes mellitus (T2DM) both in obese and normal weight individuals.
Methods We analyzed 3,479,514 metabolically healthy subjects aged over 20 years from the Korean National Health Screening Program, who underwent health examination between 2009 and 2010, with a follow-up after 4 years. The relative risk for T2DM incidence until the December 2017 was compared among the four groups: stable metabolically healthy normal weight (MHNW), unstable MHNW, stable MHO, and unstable MHO.
Results During the 4 years, 11.1% of subjects in the MHNW group, and 31.5% in the MHO group converted to a metabolically unhealthy phenotype. In the multivariate adjusted model, the unstable MHO group showed the highest risk of T2DM (hazard ratio [HR], 4.67; 95% confidence interval [CI], 4.58 to 4.77). The unstable MHNW group had a higher risk of T2DM than stable MHO group ([HR, 3.23; 95% CI, 3.16 to 3.30] vs. [HR, 1.81; 95% CI, 1.76 to 1.85]). The stable MHO group showed a higher risk of T2DM than the stable MHNW group. The influence of the transition into a metabolically unhealthy phenotype on T2DM incidence was greater in subjects with aged <65 years, women, and those with weight gain.
Conclusion Metabolically healthy phenotype was transient both in normal weight and obese individuals. Maintaining metabolic health was critical for the prevention of T2DM, irrespective of their baseline body mass index.
-
Citations
Citations to this article as recorded by- Metabolically healthy obese individuals are still at high risk for diabetes: Application of the marginal structural model
Hye Ah Lee, Hyesook Park
Diabetes, Obesity and Metabolism.2024; 26(2): 431. CrossRef - Association of anthropometric parameters as a risk factor for development of diabetic retinopathy in patients with diabetes mellitus
Aditya Verma, Ashok Jha, Ahmed Roshdy Alagorie, Rishi Sharma
Eye.2023; 37(2): 303. CrossRef - From Metabolic Syndrome to Type 2 Diabetes in Youth
Dario Iafusco, Roberto Franceschi, Alice Maguolo, Salvatore Guercio Nuzio, Antonino Crinò, Maurizio Delvecchio, Lorenzo Iughetti, Claudio Maffeis, Valeria Calcaterra, Melania Manco
Children.2023; 10(3): 516. CrossRef - Assessment of Metabolic Syndrome Risk Based on Body Size Phenotype in Korean Adults: Analysis of Community-based Cohort Data
Ji Young Kim, Youngran Yang
Research in Community and Public Health Nursing.2023; 34: 158. CrossRef - Dynamic Changes in Metabolic Status Are Associated With Risk of Ocular Motor Cranial Nerve Palsies
Daye Diana Choi, Kyung-Ah Park, Kyungdo Han, Sei Yeul Oh
Journal of Neuro-Ophthalmology.2023;[Epub] CrossRef - New metabolic health definition might not be a reliable predictor for diabetes in the nonobese Chinese population
Liying Li, Ziqiong Wang, Haiyan Ruan, Muxin Zhang, Linxia Zhou, Xin Wei, Ye Zhu, Jiafu Wei, Xiaoping Chen, Sen He
Diabetes Research and Clinical Practice.2022; 184: 109213. CrossRef - Metabolically healthy obesity: Is it really healthy for type 2 diabetes mellitus?
Qi Wu, Ming-Feng Xia, Xin Gao
World Journal of Diabetes.2022; 13(2): 70. CrossRef - Metabolically obese phenotype and its dynamic change are associated with increased carotid intima-media thickness: Results from a cohort study
Liping Yang, Xue Li, Li Wang, Shan Xu, Yanmei Lou, Fulan Hu
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(9): 2238. CrossRef - Obesity Metabolic Phenotype, Changes in Time and Risk of Diabetes Mellitus in an Observational Prospective Study on General Population
Chan Yang, Xiaowei Liu, Yuanyuan Dang, Juan Li, Jingyun Jing, Di Tian, Jiangwei Qiu, Jiaxing Zhang, Ni Yan, Xiuying Liu, Yi Zhao, Yuhong Zhang
International Journal of Public Health.2022;[Epub] CrossRef - Implications of metabolic health status and obesity on the risk of kidney cancer: A nationwide population-based cohort study
Yun Kyung Cho, Hwi Seung Kim, Joong-Yeol Park, Woo Je Lee, Ye-Jee Kim, Chang Hee Jung
Frontiers in Endocrinology.2022;[Epub] CrossRef - Metabolic health is a determining factor for incident colorectal cancer in the obese population: A nationwide population‐based cohort study
Yun Kyung Cho, Jiwoo Lee, Hwi Seung Kim, Joong‐Yeol Park, Woo Je Lee, Ye‐Jee Kim, Chang Hee Jung
Cancer Medicine.2021; 10(1): 220. CrossRef - Cumulative Exposure to Metabolic Syndrome Components and the Risk of Dementia: A Nationwide Population-Based Study
Yunjung Cho, Kyungdo Han, Da Hye Kim, Yong-Moon Park, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Endocrinology and Metabolism.2021; 36(2): 424. CrossRef - Excessive Intake of High-Fructose Corn Syrup Drinks Induces Impaired Glucose Tolerance
Hidemi Hattori, Yuma Hanai, Yuto Oshima, Hiroaki Kataoka, Nozomu Eto
Biomedicines.2021; 9(5): 541. CrossRef - The risk of Alzheimer’s disease according to dynamic changes in metabolic health and obesity: a nationwide population-based cohort study
Yun Kyung Cho, Jiwoo Lee, Hwi Seung Kim, Joong-Yeol Park, Woo Je Lee, Ye-Jee Kim, Chang Hee Jung
Aging.2021; 13(13): 16974. CrossRef - Metabolically healthy obesity: predictors of transformation to unhealthy phenotype in St Petersburg population (according to the ESSE-RF study)
M. A. Boyarinova, O. P. Rotar, A. M. Erina, N. A. Paskar, A. S. Alieva, E. V. Moguchaia, E. P. Kolesova, A. O. Konradi
"Arterial’naya Gipertenziya" ("Arterial Hypertension").2021; 27(3): 279. CrossRef - Physiological and Lifestyle Traits of Metabolic Dysfunction in the Absence of Obesity
Hanna Bjørk Klitgaard, Jesper Hoffmann Kilbak, Erica Arhnung Nozawa, Ann V. Seidel, Faidon Magkos
Current Diabetes Reports.2020;[Epub] CrossRef - Exploring Therapeutic Targets to Reverse or Prevent the Transition from Metabolically Healthy to Unhealthy Obesity
Tenzin D. Dagpo, Christopher J. Nolan, Viviane Delghingaro-Augusto
Cells.2020; 9(7): 1596. CrossRef - Prepregnancy smoking and the risk of gestational diabetes requiring insulin therapy
Mee Kyoung Kim, Kyungdo Han, Sang Youn You, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Scientific Reports.2020;[Epub] CrossRef - Obesity with and without type 2 diabetes: are there differences in obesity history, lifestyle factors or concomitant pathology?
E. A. Shestakova, Yu. I. Yashkov, O. Yu. Rebrova, M. V. Kats, M. D. Samsonova, I. I. Dedov
Obesity and metabolism.2020; 17(4): 332. CrossRef
- Metabolically healthy obese individuals are still at high risk for diabetes: Application of the marginal structural model

- Clinical Study
- Short-Term Effects of Beraprost Sodium on the Markers for Cardiovascular Risk Prediction in Type 2 Diabetic Patients with Microalbuminuria
- Yun Mi Choi, Hyuk-Sang Kwon, Kyung Mook Choi, Won-Young Lee, Eun-Gyoung Hong
- Endocrinol Metab. 2019;34(4):398-405. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.398
- 5,316 View
- 60 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background To evaluate the changes in cardiovascular risk markers including pulse wave velocity (PWV), microalbuminuria, inflammatory cytokines, and adhesion molecules after treatment with beraprost sodium (BPS) in patients with diabetic nephropathy.
Methods This was a multicenter, prospective, randomized, double-blind, placebo-controlled trial. Type 2 diabetes mellitus patients with microalbuminuria were included. The primary endpoints were changes in microalbuminuria in spot urine and PWV after BPS or placebo (PCB) treatment for 24 weeks. The secondary endpoints were changes in clinical and metabolic parameters.
Results A total of 52 patients completed the 24-week trial. Changes in PWV were not different significantly in the BPS and PCB groups (right,
P =0.16; left,P =0.11). Changes in microalbuminuria were 14.2±157.0 and 34.5±146.6 (µg/mg Cr) in the BPS and PCB groups, respectively (P =0.63). Subgroup analysis in the high blood pressure (BP) group (baseline systolic BP >120 mm Hg and diastolic BP >80 mm Hg), showed that microalbuminuria decreased by −47.6 in the BPS group compared with an increase by 116.4 (µg/mg Cr) in the PCB group (P =0.04). Also, in the large waist circumference group (>95 cm), microalbuminuria decreased significantly in the BPS group (P =0.04).Conclusion Short-term treatment of BPS for patients with diabetic nephropathy did not show significant improvement in various cardiovascular risk factors. However, BPS significantly decreased microalbuminuria in study subjects with higher cardiovascular risk such as high BP or large waist circumference.
-
Citations
Citations to this article as recorded by- Clinical efficacy of beraprost sodium in treating chronic kidney disease: A six-month prospective study
Chen Sun, Xin Wu, Xin Zhang, Shulin Li, Ruoyu Jia, Dong Sun
Heliyon.2024; 10(2): e24156. CrossRef - Clinical efficacy and safety of beraprost sodium in the treatment of nephrotic syndrome: A meta-analysis
Peng Yan, Ben Ke, Xiangdong Fang
Medicine.2023; 102(42): e34958. CrossRef - Dysregulated coagulation system links to inflammation in diabetic kidney disease
Mengyun Xiao, Donge Tang, Shaodong Luan, Bo Hu, Wenyu Gong, Wolfgang Pommer, Yong Dai, Lianghong Yin
Frontiers in Clinical Diabetes and Healthcare.2023;[Epub] CrossRef - The effects of beraprost sodium on renal function and cardiometabolic profile in patients with diabetes mellitus: a systematic review and meta-analysis of clinical trials
Peyman Nowrouzi-Sohrabi, Reza Tabrizi, Kamran Hessami, Mojtaba Shabani-Borujeni, Mahnaz Hosseini-Bensenjan, Shahla Rezaei, Mohammad Jalali, Pedram Keshavarz, Fariba Ahmadizar
International Urology and Nephrology.2022; 54(1): 111. CrossRef - Thrombocytopenia in COVID‑19 and vaccine‑induced thrombotic thrombocytopenia
Styliani Geronikolou, Işil Takan, Athanasia Pavlopoulou, Marina Mantzourani, George Chrousos
International Journal of Molecular Medicine.2022;[Epub] CrossRef - The Role of Platelets in Diabetic Kidney Disease
Ukhti Jamil Rustiasari, Joris J. Roelofs
International Journal of Molecular Sciences.2022; 23(15): 8270. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef
- Clinical efficacy of beraprost sodium in treating chronic kidney disease: A six-month prospective study

- A Case of Isolated ACTH Deficiency.
- Sang Jin Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi
- J Korean Endocr Soc. 1995;10(4):445-450. Published online November 7, 2019
- 1,098 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - solated ACTH deficiency is a very uncommon cause of hypoadrenocorticism, with less than 200 cases reported in the literatures. The clinical presentation can be similar to that of primary adrenal insufficiency, but there is a greater tendency for hypoglycemia and absence of hyperpigmentation. The diagnosis is established by demonstrating hypocortisolism with undetectable serum levels of ACTH, normal adrenal responsiveness to prolonged ACTH infusion, and an absent ACTH response to insulin-induced hypoglycemia. Other endocrine function is normal.We experienced a case of isolated ACTH deficiency in 34 years old female who was admitted due to fever and drowsy mentality.So we present this case with a review of literatures.

- A Clinical Study of 11 Cases of Adrenal Ineidentaloma.
- Jae Myung Yoo, Sang Jin Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Yong Hyun Kim, Eun Jong Lee
- J Korean Endocr Soc. 1994;9(4):358-365. Published online November 6, 2019
- 1,103 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - With the wide application of ultrasonography and CT scanning, the incidental finding of a radiologic abnormality, apparently adrenal origin, has presented a problem for clinical management. The prevalence of these clinically silent tumors has been reported as 0.6 to 1.3% of upper abdominal CT scans performed for other reasons.Once identified, an adrenal lesion must characterized as to its functional status and malignant potential. A thorough approach that initially excludes biochemical hypersecretion, then considers characteristics of anatomy and the functional nature of an adrenal mass, will allow a rational and cost-effective evaluation and management of these lesions.We present out experience of eleven adrenal incidentalomas with a review of literatures.

- Changes in Bone Mineral Density in Patients with Sheehan's Syndrome.
- Jae Myung Yoo, Sang Jin Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Eun Jong Lee, Yong Hyun Kim
- J Korean Endocr Soc. 1994;9(1):10-17. Published online November 6, 2019
- 1,469 View
- 40 Download
-
 Abstract
Abstract
 PDF
PDF - Osteoporosis is a common clinical problem with high risk of fractures in old age, especially postmenopausal women.Secondary causes of osteoporosis can be identified in 20% of women and 40% of men with vertebral fractures. One of the causes of secondary osteoporosis is endocrine disease such as hypogonadism, ovarian agenesis, hyperadrenocorticism, hyperthyroidism, hyperparathyroidism and diabetes mellitus. Patients with Sheehan's syndrome have deficiency of multiple hormones which may cause bone loss.To determine changes in the bone mineral density in women with Sheehan's syndrome and to compare clinical and biochemical characteristics between the patients with osteoporosis and the patients without osteoporosis, we measured the bone mineral density(BMD) of the lumber spine and midradius by dual energy X-ray absortiometry(DEXA) and the serum levels of estrogen and osteocalcin in 11 patients of Sheehan's syndrome.The results were as follows;1) The BMDs of the lumbar spine were significantly decreased in patients with Sheehan's syndrome when compared with those of age-matched control.2) The prevalence of osteoporosis in patients with Sheehan's syndromes was 55%. Between the patients with osteoporosis and the patients without osteoporosis, there were no difference in the onset age of amenorrhea, the duration of amenorrhea, and the serum levels of osteocalcin and alkaline phosphatase.3) Serum estradiol levels were decreased uniformly in the patients with Sheehan's syndrome except three patients with estrogen replacement, but the concentration of estradiol was not correlated with the degree of the decrease in bone mass.In conclusion, the patients with Sheehan's syndrome have an increased prevalence of osteoporosis. But the effect of each anterior pituitary hormone deficiency on bone loss should be clarified in the futher prospective study.

- Effects of Vildagliptin or Pioglitazone on Glycemic Variability and Oxidative Stress in Patients with Type 2 Diabetes Inadequately Controlled with Metformin Monotherapy: A 16-Week, Randomised, Open Label, Pilot Study
- Nam Hoon Kim, Dong-Lim Kim, Kyeong Jin Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim
- Endocrinol Metab. 2017;32(2):241-247. Published online June 23, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.2.241
- 4,639 View
- 94 Download
- 23 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Glycemic variability is associated with the development of diabetic complications through the activation of oxidative stress. This study aimed to evaluate the effects of a dipeptidyl peptidase 4 inhibitor, vildagliptin, or a thiazolidinedione, pioglitazone, on glycemic variability and oxidative stress in patients with type 2 diabetes.
Methods In this open label, randomised, active-controlled, pilot trial, individuals who were inadequately controlled with metformin monotherapy were assigned to either vildagliptin (50 mg twice daily,
n =17) or pioglitazone (15 mg once daily,n =14) treatment groups for 16 weeks. Glycemic variability was assessed by calculating the mean amplitude of glycemic excursions (MAGE), which was obtained from continuous glucose monitoring. Urinary 8-iso prostaglandin F2α, serum oxidised low density lipoprotein, and high-sensitivity C-reactive protein were used as markers of oxidative stress or inflammation.Results Both vildagliptin and pioglitazone significantly reduced glycated hemoglobin and mean plasma glucose levels during the 16-week treatment. Vildagliptin also significantly reduced the MAGE (from 93.8±38.0 to 70.8±19.2 mg/dL,
P =0.046), and mean standard deviation of 24 hours glucose (from 38±17.3 to 27.7±6.9,P =0.026); however, pioglitazone did not, although the magnitude of decline was similar in both groups. Markers of oxidative stress or inflammation including urinary 8-iso prostaglandin F2α did not change after treatment in both groups.Conclusion In this 16-week treatment trial, vildagliptin, but not pioglitazone, reduced glycemic variability in individuals with type 2 diabetes who was inadequately controlled with metformin monotherapy, although a reduction of oxidative stress markers was not observed.
-
Citations
Citations to this article as recorded by- What is Glycaemic Variability and which Pharmacological Treatment Options are Effective? A Narrative Review
Juan Miguel Huertas Cañas, Maria Alejandra Gomez Gutierrez, Andres Bedoya Ossa
European Endocrinology.2023; 19(2): 4. CrossRef - Glycemic Variability, Glycated Hemoglobin, and Cardiovascular Complications: Still a Dilemma in Clinical Practice
Antonio Ceriello, Ali A. Rizvi, Manfredi Rizzo
Advances in Therapy.2022; 39(1): 1. CrossRef - Contrasting Three Non-hypoglycemic Antidiabetic Drug Effects on Glycemic Control in Newly Diagnosed Type II Diabetes Mellitus: An Experimental Study
Abdulhamza Hmood, Mohammed Almasoody, Hameed Hussein Al-Jameel
Open Access Macedonian Journal of Medical Sciences.2022; 10(B): 506. CrossRef - Hypoglycemic agents and glycemic variability in individuals with type 2 diabetes: A systematic review and network meta-analysis
SuA Oh, Sujata Purja, Hocheol Shin, Minji Kim, Eunyoung Kim
Diabetes and Vascular Disease Research.2022; 19(3): 147916412211068. CrossRef - Influence of dipeptidyl peptidase-4 inhibitors on glycemic variability in patients with type 2 diabetes: A meta-analysis of randomized controlled trials
Shangyu Chai, Ruya Zhang, Ye Zhang, Richard David Carr, Yiman Zheng, Swapnil Rajpathak, Miao Yu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Comparison of Efficacy of Glimepiride, Alogliptin, and Alogliptin-Pioglitazone as the Initial Periods of Therapy in Patients with Poorly Controlled Type 2 Diabetes Mellitus: An Open-Label, Multicenter, Randomized, Controlled Study
Hae Jin Kim, In Kyung Jeong, Kyu Yeon Hur, Soo-Kyung Kim, Jung Hyun Noh, Sung Wan Chun, Eun Seok Kang, Eun-Jung Rhee, Sung Hee Choi
Diabetes & Metabolism Journal.2022; 46(5): 689. CrossRef - Effect of low dose allopurinol on glycemic control and glycemic variability in patients with type 2 diabetes mellitus: A cross-sectional study
Manal M. Alem
Heliyon.2022; 8(11): e11549. CrossRef - Effect of hydroxychloroquine on glycemic variability in type 2 diabetes patients uncontrolled on glimepiride and metformin therapy
Rajesh Rajput, Suyasha Saini, Siddhant Rajput, Parankush Upadhyay
Indian Journal of Endocrinology and Metabolism.2022; 26(6): 537. CrossRef - Effect of Dapagliflozin as an Add-on Therapy to Insulin on the Glycemic Variability in Subjects with Type 2 Diabetes Mellitus (DIVE): A Multicenter, Placebo-Controlled, Double-Blind, Randomized Study
Seung-Hwan Lee, Kyung-Wan Min, Byung-Wan Lee, In-Kyung Jeong, Soon-Jib Yoo, Hyuk-Sang Kwon, Yoon-Hee Choi, Kun-Ho Yoon
Diabetes & Metabolism Journal.2021; 45(3): 339. CrossRef - Comprehensive elaboration of glycemic variability in diabetic macrovascular and microvascular complications
Bao Sun, Zhiying Luo, Jiecan Zhou
Cardiovascular Diabetology.2021;[Epub] CrossRef - CGMS and Glycemic Variability, Relevance in Clinical Research to Evaluate Interventions in T2D, a Literature Review
Anne-Esther Breyton, Stéphanie Lambert-Porcheron, Martine Laville, Sophie Vinoy, Julie-Anne Nazare
Frontiers in Endocrinology.2021;[Epub] CrossRef - Efficacy and safety profile of sitagliptin, vildagliptin, and metformin in newly diagnosed type 2 diabetic subjects
Sahar Hossam Elhini, Amal K. Hussien, Ahmed Abd Elsamie Omran, Asmaa A. Elsayed, Haitham saeed
Clinical and Experimental Pharmacology and Physiology.2021; 48(12): 1589. CrossRef - Vildagliptin ameliorates renal injury in type 2 diabetic rats by suppressing oxidative stress
Fariba Aghahoseini, Alireza Alihemmati, Leila Hosseini, Reza Badalzadeh
Journal of Diabetes & Metabolic Disorders.2020; 19(2): 701. CrossRef - Small changes in glucose variability induced by low and high glycemic index diets are not associated with changes in β-cell function in adults with pre-diabetes
Kristina M. Utzschneider, Tonya N. Johnson, Kara L. Breymeyer, Lisa Bettcher, Daniel Raftery, Katherine M. Newton, Marian L. Neuhouser
Journal of Diabetes and its Complications.2020; 34(8): 107586. CrossRef - Comparison of the effects of gemigliptin and dapagliflozin on glycaemic variability in type 2 diabetes: A randomized, open‐label, active‐controlled, 12‐week study (STABLE II study)
Soo Heon Kwak, You‐Cheol Hwang, Jong Chul Won, Ji Cheol Bae, Hyun Jin Kim, Sunghwan Suh, Eun Young Lee, Subin Lee, Sang‐Yong Kim, Jae Hyeon Kim
Diabetes, Obesity and Metabolism.2020; 22(2): 173. CrossRef - Glycemic variability: adverse clinical outcomes and how to improve it?
Zheng Zhou, Bao Sun, Shiqiong Huang, Chunsheng Zhu, Meng Bian
Cardiovascular Diabetology.2020;[Epub] CrossRef - Anti-inflammatory properties of antidiabetic drugs: A “promised land” in the COVID-19 era?
Niki Katsiki, Ele Ferrannini
Journal of Diabetes and its Complications.2020; 34(12): 107723. CrossRef - Impact of long-term glucose variability on coronary atherosclerosis progression in patients with type 2 diabetes: a 2.3 year follow-up study
Suhua Li, Xixiang Tang, Yanting Luo, Bingyuan Wu, Zhuoshan Huang, Zexiong Li, Long Peng, Yesheng Ling, Jieming Zhu, Junlin Zhong, Jinlai Liu, Yanming Chen
Cardiovascular Diabetology.2020;[Epub] CrossRef - Visit-to-visit fasting plasma glucose variability is an important risk factor for long-term changes in left cardiac structure and function in patients with type 2 diabetes
Xixiang Tang, Junlin Zhong, Hui Zhang, Yanting Luo, Xing Liu, Long Peng, Yanling Zhang, Xiaoxian Qian, Boxiong Jiang, Jinlai Liu, Suhua Li, Yanming Chen
Cardiovascular Diabetology.2019;[Epub] CrossRef - Effect of dipeptidyl-peptidase-4 inhibitors on C-reactive protein in patients with type 2 diabetes: a systematic review and meta-analysis
Xin Liu, Peng Men, Bo Wang, Gaojun Cai, Zhigang Zhao
Lipids in Health and Disease.2019;[Epub] CrossRef - Efficacy and Safety of Pioglitazone Monotherapy in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomised Controlled Trials
Fahmida Alam, Md. Asiful Islam, Mafauzy Mohamed, Imran Ahmad, Mohammad Amjad Kamal, Richard Donnelly, Iskandar Idris, Siew Hua Gan
Scientific Reports.2019;[Epub] CrossRef - Effect of DPP-IV Inhibitors on Glycemic Variability in Patients with T2DM: A Systematic Review and Meta-Analysis
Subin Lee, Heeyoung Lee, Yoonhye Kim, EunYoung Kim
Scientific Reports.2019;[Epub] CrossRef - Glycemic Variability: How to Measure and Its Clinical Implication for Type 2 Diabetes
Guillermo E. Umpierrez, Boris P. Kovatchev
The American Journal of the Medical Sciences.2018; 356(6): 518. CrossRef
- What is Glycaemic Variability and which Pharmacological Treatment Options are Effective? A Narrative Review

- Obesity and Metabolism
- The Impact of Organokines on Insulin Resistance, Inflammation, and Atherosclerosis
- Kyung Mook Choi
- Endocrinol Metab. 2016;31(1):1-6. Published online March 16, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.1.1
- 4,932 View
- 66 Download
- 39 Web of Science
- 42 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Immoderate energy intake, a sedentary lifestyle, and aging have contributed to the increased prevalence of obesity, sarcopenia, metabolic syndrome, type 2 diabetes, and cardiovascular disease. There is an urgent need for the development of novel pharmacological interventions that can target excessive fat accumulation and decreased muscle mass and/or strength. Adipokines, bioactive molecules derived from adipose tissue, are involved in the regulation of appetite and satiety, inflammation, energy expenditure, insulin resistance and secretion, glucose and lipid metabolism, and atherosclerosis. Recently, there is emerging evidence that skeletal muscle and the liver also function as endocrine organs that secrete myokines and hepatokines, respectively. Novel discoveries and research into these organokines (adipokines, myokines, and hepatokines) may lead to the development of promising biomarkers and therapeutics for cardiometabolic disease. In this review, I summarize recent data on these organokines and focus on the role of adipokines, myokines, and hepatokines in the regulation of insulin resistance, inflammation, and atherosclerosis.
-
Citations
Citations to this article as recorded by- Cardiometabolic diseases and early cognitive decline: Mitigated by integrated active lifestyle for brain health
Haowei Li, Shige Qi, Shengshu Wang, Shanshan Yang, Shaohua Liu, Shimin Chen, Xuehang Li, Rongrong Li, Junhan Yang, Huaihao Li, Yinghui Bao, Yueting Shi, Zhihui Wang, Miao Liu, Yao He
Journal of Affective Disorders.2024; 350: 155. CrossRef - Current status and future perspectives of FGF21 analogues in clinical trials
Zara Siu Wa Chui, Qing Shen, Aimin Xu
Trends in Endocrinology & Metabolism.2024;[Epub] CrossRef - Organokinler ve Biyokimyasal Etkileri
Ahmet İlhan, Umut Kökbaş
Arşiv Kaynak Tarama Dergisi.2024; 33(1): 71. CrossRef - The Significance of Selected Myokines in Predicting the Length of Rehabilitation of Patients after COVID-19 Infection
Alicja Mińko, Agnieszka Turoń-Skrzypińska, Aleksandra Rył, Katarzyna Mańkowska, Aneta Cymbaluk-Płoska, Iwona Rotter
Biomedicines.2024; 12(4): 836. CrossRef - Pathophysiology of type 2 diabetes and the impact of altered metabolic interorgan crosstalk
Jose Marcos Sanches, Li Na Zhao, Albert Salehi, Claes B. Wollheim, Philipp Kaldis
The FEBS Journal.2023; 290(3): 620. CrossRef - Research Progress on the Mechanism of Obesity-Induced Cardiovascular Disease
文清 刘
Advances in Clinical Medicine.2023; 13(08): 12887. CrossRef - The Pan-liver Network Theory: From Traditional Chinese Medicine to Western Medicine
Yaxing Zhang, Xian-Ming Fang
Chinese Journal of Physiology.2023; 66(6): 401. CrossRef - Higher serum level of CTRP15 in patients with coronary artery disease is associated with disease severity, body mass index and insulin resistance
Abolfazl Shokoohi Nahrkhalaji, Reza Ahmadi, Reza Fadaei, Ghodratollah Panahi, Malihe Razzaghi, Soudabeh Fallah
Archives of Physiology and Biochemistry.2022; 128(1): 276. CrossRef - Non-Alcoholic Steatohepatitis (NASH) and Organokines: What Is Now and What Will Be in the Future
João Paulo Margiotti dos Santos, Mariana Canevari de Maio, Monike Alves Lemes, Lucas Fornari Laurindo, Jesselina Francisco dos Santos Haber, Marcelo Dib Bechara, Pedro Sidnei do Prado, Eduardo Costa Rauen, Fernando Costa, Barbara Cristina de Abreu Pereira
International Journal of Molecular Sciences.2022; 23(1): 498. CrossRef - Hepatic PTEN Signaling Regulates Systemic Metabolic Homeostasis through Hepatokines-Mediated Liver-to-Peripheral Organs Crosstalk
Flavien Berthou, Cyril Sobolewski, Daniel Abegg, Margot Fournier, Christine Maeder, Dobrochna Dolicka, Marta Correia de Sousa, Alexander Adibekian, Michelangelo Foti
International Journal of Molecular Sciences.2022; 23(7): 3959. CrossRef - Non-Alcoholic Fatty Liver Disease and Metabolic Syndrome in Women: Effects of Lifestyle Modifications
Maria Teresa Guagnano, Damiano D'Ardes, Rossi Ilaria, Francesca Santilli, Cosima Schiavone, Marco Bucci, Francesco Cipollone
Journal of Clinical Medicine.2022; 11(10): 2759. CrossRef - Contribution of organokines in the development of NAFLD/NASH associated hepatocellular carcinoma
Meenakshi Vachher, Savita Bansal, Bhupender Kumar, Sandeep Yadav, Taruna Arora, Nalini Moza Wali, Archana Burman
Journal of Cellular Biochemistry.2022; 123(10): 1553. CrossRef - Organokines, Sarcopenia, and Metabolic Repercussions: The Vicious Cycle and the Interplay with Exercise
Giulia Minniti, Letícia Maria Pescinini-Salzedas, Guilherme Almeida dos Santos Minniti, Lucas Fornari Laurindo, Sandra Maria Barbalho, Renata Vargas Sinatora, Lance Alan Sloan, Rafael Santos de Argollo Haber, Adriano Cressoni Araújo, Karina Quesada, Jesse
International Journal of Molecular Sciences.2022; 23(21): 13452. CrossRef - CURRENT CONCEPTS ON LEPTIN-MEDIATED REGULATION OF METABOLISM
R. B. Aliiev
Bulletin of Problems Biology and Medicine.2022; 1(4): 9-1. CrossRef - Inflammatory biomarkers and prediction of insulin resistance in Congolese adults
Reine Freudlendrich Eboka-Loumingou Sakou, Benjamin Longo-Mbenza, Mûnka Nkalla-Lambi, Etienne Mokondjimobe, Henry Germain Monabeka, Donatien Moukassa, Ange Antoine Abena, Mia Pamela Mekieje Tumchou, Venant Tchokonte-Nana
Heliyon.2021; 7(2): e06139. CrossRef - Adipokines, Myokines, and Hepatokines: Crosstalk and Metabolic Repercussions
Ana Rita de Oliveira dos Santos, Bárbara de Oliveira Zanuso, Vitor Fernando Bordin Miola, Sandra Maria Barbalho, Patrícia C. Santos Bueno, Uri Adrian Prync Flato, Claudia Rucco P. Detregiachi, Daniela Vieira Buchaim, Rogério Leone Buchaim, Ricardo José To
International Journal of Molecular Sciences.2021; 22(5): 2639. CrossRef - The Effects of Two Different Intensities of Combined Training on C1q/TNF-Related Protein 3 (CTRP3) and Insulin Resistance in Women with Non-alcoholic Fatty Liver Disease
Somayeh Rajabi, Roya Askari, Amir Hossein Haghighi, Nasrin Razavianzadeh
Hepatitis Monthly.2021;[Epub] CrossRef - Handgrip and sex-specific cardiometabolic risk factors in Hispanic/Latino migrant farmworkers
Anas Raed, Jessica Bilz, Miriam Cortez-Cooper, Lufei Young, Li Chen, Pamela Cromer, Haidong Zhu, Andrew Mazzoli, Samip Parikh, Jigar Bhagatwala, Yutong Dong, Zhuo Sun, Debbie Layman, Yanbin Dong
Scientific Reports.2021;[Epub] CrossRef - Crossing the Antarctica: Exploring the Effects of Appetite-Regulating Hormones and Indicators of Nutrition Status during a 93-Day Solo-Expedition
Bjørn Helge Johnsen, Guttorm Brattebø, Terry M. Phillips, Rune Gjeldnes, Paul T. Bartone, Hans-Olav Neteland Monsen, Julian F. Thayer
Nutrients.2021; 13(6): 1777. CrossRef - Irisin in atherosclerosis
Zhe-Bin Cheng, Liang Huang, Xuan Xiao, Jia-Xiang Sun, Zi-Kai Zou, Jie-Feng Jiang, Cong Lu, Hai-Ya Zhang, Chi Zhang
Clinica Chimica Acta.2021; 522: 158. CrossRef - Pilates and TRX training methods can improve insulin resistance in overweight women by increasing an exercise-hormone, Irisin
Marzyeh Rahimi, Parvaneh Nazarali, Rostam Alizadeh
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1455. CrossRef - Effects of GLP-1 receptor agonists on myokine levels and pro-inflammatory cytokines in patients with type 2 diabetes mellitus
Valentina Guarnotta, Maria J. Bianco, Enrica Vigneri, Felicia Panto’, Bruna Lo Sasso, Marcello Ciaccio, Giuseppe Pizzolanti, Carla Giordano
Nutrition, Metabolism and Cardiovascular Diseases.2021; 31(11): 3193. CrossRef - Hepatokines and Non-Alcoholic Fatty Liver Disease: Linking Liver Pathophysiology to Metabolism
Tae Hyun Kim, Dong-Gyun Hong, Yoon Mee Yang
Biomedicines.2021; 9(12): 1903. CrossRef - Higher circulating levels of ANGPTL8 are associated with body mass index, triglycerides, and endothelial dysfunction in patients with coronary artery disease
Reza Fadaei, Hossein Shateri, Johanna K. DiStefano, Nariman Moradi, Mohammad Mohammadi, Farzad Emami, Hassan Aghajani, Nasrin Ziamajidi
Molecular and Cellular Biochemistry.2020; 469(1-2): 29. CrossRef - Nonalcoholic fatty liver disease and cardiovascular disease phenotypes
Giandomenico Bisaccia, Fabrizio Ricci, Cesare Mantini, Claudio Tana, Gian Luca Romani, Cosima Schiavone, Sabina Gallina
SAGE Open Medicine.2020; 8: 205031212093380. CrossRef - Dysregulated Autophagy Mediates Sarcopenic Obesity and Its Complications via AMPK and PGC1α Signaling Pathways: Potential Involvement of Gut Dysbiosis as a Pathological Link
Ji Yeon Ryu, Hyung Muk Choi, Hyung-In Yang, Kyoung Soo Kim
International Journal of Molecular Sciences.2020; 21(18): 6887. CrossRef - Fetuin-A as a Potential Biomarker of Metabolic Variability Following 60 Days of Bed Rest
Kiera Ward, Edwin Mulder, Petra Frings-Meuthen, Donal J. O’Gorman, Diane Cooper
Frontiers in Physiology.2020;[Epub] CrossRef - Effect of Moderate Aerobic Exercise on Serum Levels of FGF21 and Fetuin A in Women with Type 2 Diabetes
Exir Vizvari, Parvin farzanegi, Hajar Abbas Zade
Medical Laboratory Journal.2020; 14(6): 17. CrossRef - The implication of hepatokines in metabolic syndrome
Maryam Esfahani, Mostafa Baranchi, Mohammad Taghi Goodarzi
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(4): 2477. CrossRef - The Role of Adipose Tissue and Adipokines in Sepsis: Inflammatory and Metabolic Considerations, and the Obesity Paradox
Irene Karampela, Gerasimos Socrates Christodoulatos, Maria Dalamaga
Current Obesity Reports.2019; 8(4): 434. CrossRef - Sarcopenia and myokines profile as risk factors in cardiovascular diseases?
Mariusz Ciołkiewicz, Anna Kuryliszyn-Moskal, Anna Hryniewicz, Karol Kamiński
Postępy Higieny i Medycyny Doświadczalnej.2019; 73: 550. CrossRef - Pathophysiological Implication of Fetuin-A Glycoprotein in the Development of Metabolic Disorders: A Concise Review
Lynda Bourebaba, Krzysztof Marycz
Journal of Clinical Medicine.2019; 8(12): 2033. CrossRef - Loss of Glycine N-Methyltransferase Associates with Angiopoietin-Like Protein 8 Expression in High Fat-Diet-Fed Mice
Jian-Wei Huang, Chao-Ju Chen, Chia-Hung Yen, Yi-Ming Arthur Chen, Yu-Peng Liu
International Journal of Molecular Sciences.2019; 20(17): 4223. CrossRef - Recent advances in biosensor technology in assessment of early diabetes biomarkers
Armin Salek-Maghsoudi, Faezeh Vakhshiteh, Raheleh Torabi, Shokoufeh Hassani, Mohammad Reza Ganjali, Parviz Norouzi, Morteza Hosseini, Mohammad Abdollahi
Biosensors and Bioelectronics.2018; 99: 122. CrossRef - Insulin-stimulated glucose uptake in skeletal muscle, adipose tissue and liver: a positron emission tomography study
Miikka-Juhani Honka, Aino Latva-Rasku, Marco Bucci, Kirsi A Virtanen, Jarna C Hannukainen, Kari K Kalliokoski, Pirjo Nuutila
European Journal of Endocrinology.2018; 178(5): 523. CrossRef - Magnetic multiwalled carbon nanotubes as nanocarrier tags for sensitive determination of fetuin in saliva
Esther Sánchez-Tirado, Araceli González-Cortés, Paloma Yáñez-Sedeño, José M. Pingarrón
Biosensors and Bioelectronics.2018; 113: 88. CrossRef - Decreased muscle mass in Korean subjects with intracranial arterial stenosis: The Kangbuk Samsung Health Study
Ho-Jung Jung, Hwanseok Jung, Taeyoung Lee, Jongho Kim, Jongsin Park, Hacsoo Kim, Junghwan Cho, Won-Young Lee, Sung-Woo Park, Eun-Jung Rhee, Hyung-Geun Oh
Atherosclerosis.2017; 256: 89. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Low muscle mass and risk of type 2 diabetes in middle-aged and older adults: findings from the KoGES
Jang Won Son, Seong Su Lee, Sung Rae Kim, Soon Jib Yoo, Bong Yun Cha, Ho Young Son, Nam H. Cho
Diabetologia.2017; 60(5): 865. CrossRef - Effects of chlorogenic acid on intracellular calcium regulation in lysophosphatidylcholine-treated endothelial cells
Hye-Jin Jung, Seung-Soon Im, Dae-Kyu Song, Jae-Hoon Bae
BMB Reports.2017; 50(6): 323. CrossRef - Irisin: A Potential Link between Physical Exercise and Metabolism—An Observational Study in Differently Trained Subjects, from Elite Athletes to Sedentary People
Stefano Benedini, Elena Dozio, Pietro Luigi Invernizzi, Elena Vianello, Giuseppe Banfi, Ileana Terruzzi, Livio Luzi, Massimiliano Marco Corsi Romanelli
Journal of Diabetes Research.2017; 2017: 1. CrossRef - Serum Vaspin Concentration in Elderly Type 2 Diabetes Mellitus Patients with Differing Body Mass Index: A Cross-Sectional Study
Wei Yang, Yun Li, Tian Tian, Li Wang
BioMed Research International.2017; 2017: 1. CrossRef
- Cardiometabolic diseases and early cognitive decline: Mitigated by integrated active lifestyle for brain health

- Obesity and Metabolism
- Sarcopenia and Sarcopenic Obesity
- Kyung Mook Choi
- Endocrinol Metab. 2013;28(2):86-89. Published online June 18, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.2.86
- 5,215 View
- 59 Download
- 64 Web of Science
- 70 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The aging process is associated with progressive loss of muscle mass and strength, as well as decline in physical functioning. Although consensus diagnosis has not been reached, sarcopenia is increasingly defined by both loss of muscle mass and loss of muscle function or strength. The cause of sarcopenia is suggested as multifactorial, including hormonal changes, inflammatory pathway activation, fatty infiltration, poor nutrition, and decreased physical activity. Sarcopenia is often associated with visceral obesity. Sarcopenic obesity in the elderly impacts metabolic complications and represents a major public health challenge in a rapidly aging society. Further research about sarcopenia and sarcopenic obesity may be needed to confront the influence of aging society in Korea.
-
Citations
Citations to this article as recorded by- Influence of Sugar-Sweetened Beverages Intake on Sarcopenic Obesity, Visceral Obesity, and Sarcopenia in Lebanese Patients with MASLD: A Case-Control Study
Maha Hoteit, Myriam Dagher, Nikolaos Tzenios, Najat Al Kaaki, Ghadir Rkein, Abdul Rahman Chahine, Yonna Sacre, Samer Hotayt, Rami Matar, Mahmoud Hallal, Micheal Maitar, Bilal Hotayt
Healthcare.2024; 12(5): 591. CrossRef - Association between sarcopenia and hearing impairment in middle-aged and elderly people in China: a prospective cohort study
Zeqi Zhang
Scientific Reports.2024;[Epub] CrossRef - Sex-Specific Effects of Dietary Factors on Sarcopenic Obesity in Korean Elderly: A Nationwide Cross-Sectional Study
Soojeong Kim, Kyung Hee Hong
Nutrients.2024; 16(8): 1175. CrossRef - Aging, Physical Exercise, Telomeres, and Sarcopenia: A Narrative Review
David Hernández-Álvarez, Juana Rosado-Pérez, Graciela Gavia-García, Taide Laurita Arista-Ugalde, Itzen Aguiñiga-Sánchez, Edelmiro Santiago-Osorio, Víctor Manuel Mendoza-Núñez
Biomedicines.2023; 11(2): 598. CrossRef - Interplay of skeletal muscle and adipose tissue: sarcopenic obesity
Min Jeong Park, Kyung Mook Choi
Metabolism.2023; 144: 155577. CrossRef - Sarcopenia in chronic kidney disease: from bench to bedside
Da Woon Kim, Sang Heon Song
The Korean Journal of Internal Medicine.2023; 38(3): 303. CrossRef - The serum creatinine to cystatin C to waist circumference ratios predicts risk for type 2 diabetes: A Chinese cohort study
Yinfei Chen, Weiheng Wen, Zhiliang Mai, Ming Wang, Hong Chen, Jia Sun
Journal of Diabetes.2023; 15(10): 808. CrossRef - Sarcopenic obesity in children
A. N. Zav’yalova, M. E. Troshkina, L. A. Shcherbak, V. P. Novikova
Experimental and Clinical Gastroenterology.2023; 1(1): 134. CrossRef - The Effects of Obesity on the Inflammatory, Cardiovascular, and Neurobiological Responses to Exercise in Older Adults
Brandon G. Fico, Arun Maharaj, Gabriel S. Pena, Chun-Jung Huang
Biology.2023; 12(6): 865. CrossRef - Correlation of Sarcopenic Obesity on Various Cardiometabolic Risk Factors and Fracture Risk in Mid-Aged Korean Women
Eun Hee Yu, Hyun Joo Lee, Hyeon Jin Kim, In Hye Kim, Jong Kil Joo, Yong Jin Na
Journal of Menopausal Medicine.2023; 29(2): 58. CrossRef - Sarkopenik Obezite ile Mücadelede Egzersiz ve Beslenme Stratejileri
Ayşe ŞİMŞEK, Musa GÜNEŞ, Büşra DEMİRER
İstanbul Gelişim Üniversitesi Sağlık Bilimleri Dergisi.2023; (20): 677. CrossRef - How to Diagnose Sarcopenic Obesity in Candidates for Bariatric Surgery?
Gabriela B. Bacelar, Estevão F. Sampaio, Wagno Alcântara, João Gabriel Lustoza, Cláudia Daltro, Carla Daltro
Bariatric Surgical Practice and Patient Care.2022; 17(4): 237. CrossRef - Usefulness of Muscle Ultrasound to Study Sarcopenic Obesity: A Pilot Case-Control Study
Andreu Simó-Servat, Montse Ibarra, Mireia Libran, Silvia Rodríguez, Verónica Perea, Carmen Quirós, Aida Orois, Noelia Pérez, Rafael Simó, Maria-José Barahona
Journal of Clinical Medicine.2022; 11(10): 2886. CrossRef - Association between body shape index and risk of mortality in the United States
Heysoo Lee, Hye Soo Chung, Yoon Jung Kim, Min Kyu Choi, Yong Kyun Roh, Wankyo Chung, Jae Myung Yu, Chang-Myung Oh, Shinje Moon
Scientific Reports.2022;[Epub] CrossRef - Associations between Weight-Adjusted Waist Index and Abdominal Fat and Muscle Mass: Multi-Ethnic Study of Atherosclerosis
Ji Yoon Kim, Jimi Choi, Chantal A. Vella, Michael H. Criqui, Matthew A. Allison, Nam Hoon Kim
Diabetes & Metabolism Journal.2022; 46(5): 747. CrossRef - Prevalence of Sarcopenic Obesity in Various Comorbidities, Diagnostic Markers, and Therapeutic Approaches: A Review
Mangalam Kumari, Archana Khanna
Annals of Geriatric Medicine and Research.2022; 26(4): 296. CrossRef - Sarcopenic obesity: research advances in pathogenesis and diagnostic criteria
Wen-qing Xie, Ge-lei Xiao, Yi-bin Fan, Miao He, Shan Lv, Yu-sheng Li
Aging Clinical and Experimental Research.2021; 33(2): 247. CrossRef - Effect of Sarcopenia and Body Shape on Cardiovascular Disease According to Obesity Phenotypes
Hyun-Woong Cho, Wankyo Chung, Shinje Moon, Ohk-Hyun Ryu, Min Kyung Kim, Jun Goo Kang
Diabetes & Metabolism Journal.2021; 45(2): 209. CrossRef - Prevalence, diagnostic criteria, and factors associated with sarcopenic obesity in older adults from a low middle income country: A systematic review
Maria Sortênia Alves Guimarães, Carolina Araújo dos Santos, Joice da Silva Castro, Leidjaira Lopes Juvanhol, Fabiane Aparecida Canaan Rezende, Karina Oliveira Martinho, Andréia Queiroz Ribeiro
Clinical Nutrition ESPEN.2021; 41: 94. CrossRef - Engagement in Muscle-Strengthening Activities Lowers Sarcopenia Risk in Older Adults Already Adhering to the Aerobic Physical Activity Guidelines
Jort Veen, Diego Montiel-Rojas, Andreas Nilsson, Fawzi Kadi
International Journal of Environmental Research and Public Health.2021; 18(3): 989. CrossRef - Effect of CCL11 on In Vitro Myogenesis and Its Clinical Relevance for Sarcopenia in Older Adults
Da Ae Kim, So Jeong Park, Jin Young Lee, Jeoung Hee Kim, Seungjoo Lee, Eunju Lee, Il-Young Jang, Hee-Won Jung, Jin Hoon Park, Beom-Jun Kim
Endocrinology and Metabolism.2021; 36(2): 455. CrossRef - The Critical Role of Oxidative Stress in Sarcopenic Obesity
Andrea Gonzalez, Felipe Simon, Oscar Achiardi, Cristian Vilos, Daniel Cabrera, Claudio Cabello-Verrugio, Vladimir Jakovljevic
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - Evaluation of the association between decreased skeletal muscle mass and extubation failure after long-term mechanical ventilation
Hye Young Woo, Seung-Young Oh, Hannah Lee, Ho Geol Ryu
Clinical Nutrition.2020; 39(9): 2764. CrossRef - Association Between Sarcopenic Obesity and Metabolic Syndrome in Adults: A Systematic Review and Meta-Analysis
Dima Khadra, Leila Itani, Yomna Chebaro, May Obeid, Miryam Jaber, Reham Ghanem, Agnes Ayton, Dima Kreidieh, Dana E. Masri, Akira Kimura, Hana Tannir, Marwan El Ghoch
Current Cardiology Reviews.2020; 16(2): 153. CrossRef - Sarcopenic obesity in ageing: cardiovascular outcomes and mortality
Janice L. Atkins, S. Goya Wannamathee
British Journal of Nutrition.2020; 124(10): 1102. CrossRef - Inflammation and metabolism: the role of adiposity in sarcopenic obesity
G. M. Lynch, C. H. Murphy, E. de Marco Castro, H. M. Roche
Proceedings of the Nutrition Society.2020; 79(4): 435. CrossRef - Diabetes and Sarcopenic Obesity: Pathogenesis, Diagnosis, and Treatments
Mina Wang, Yan Tan, Yifan Shi, Xu Wang, Zehuan Liao, Peng Wei
Frontiers in Endocrinology.2020;[Epub] CrossRef - Relationship between Decreased Estimated Glomerular Filtration Rate and Sarcopenic Obesity among Postmenopausal Women: Korea National Health and Nutrition Examination Survey (2008–2011)
Changbin Hong, Jae Yong Baek, Ji Won Lee, Ji Hoon Lee, Kayoung Lee, Tae-jin Park, Jinseung Kim
Korean Journal of Family Medicine.2020; 41(5): 332. CrossRef - Effect of body shape on the development of cardiovascular disease in individuals with metabolically healthy obesity
Chang-Myung Oh, Jung Hwan Park, Hye Soo Chung, Jae Myung Yu, Wankyo Chung, Jun Goo Kang, Shinje Moon
Medicine.2020; 99(38): e22036. CrossRef - Sarcopenia Associated with Chronic Obstructive Pulmonary Disease
Sang Hun Kim, Myung Jun Shin, Yong Beom Shin, Ki Uk Kim
Journal of Bone Metabolism.2019; 26(2): 65. CrossRef - Sarcopenia and Sarcopenic Obesity as Novel Risk Factors for Gastric Carcinogenesis: A Health Checkup Cohort Study
Young Min Kim, Jie-Hyun Kim, Su Jung Baik, Jaeyoung Chun, Young Hoon Youn, Hyojin Park
Frontiers in Oncology.2019;[Epub] CrossRef - Association between skeletal muscle attenuation and gastroesophageal reflux disease: A health check-up cohort study
Young Min Kim, Jie-Hyun Kim, Su Jung Baik, Da Hyun Jung, Jae Jun Park, Young Hoon Youn, Hyojin Park
Scientific Reports.2019;[Epub] CrossRef - A High Serum Cortisol/DHEA-S Ratio Is a Risk Factor for Sarcopenia in Elderly Diabetic Patients
Ikumi Yanagita, Yuya Fujihara, Yuichi Kitajima, Misuzu Tajima, Masanao Honda, Tomoko Kawajiri, Terumi Eda, Kazue Yonemura, Noriko Yamaguchi, Hideko Asakawa, Yukiko Nei, Yumi Kayashima, Mihoko Yoshimoto, Mayumi Harada, Yuhei Araki, Shoji Yoshimoto, Eiji Ai
Journal of the Endocrine Society.2019; 3(4): 801. CrossRef - SARCOPENIA AND SEVERITY OF NON-ALCOHOLIC FATTY LIVER DISEASE
Josilda Ferreira CRUZ, Yasmim Anayr Costa FERRARI, Carla Perez MACHADO, Nathalia Nascimento SANTANA, Allan Victor Hora MOTA, Sonia Oliveira LIMA
Arquivos de Gastroenterologia.2019; 56(4): 357. CrossRef - Association between sarcopenic obesity and higher risk of type 2 diabetes in adults: A systematic review and meta-analysis
Dima Khadra, Leila Itani, Hana Tannir, Dima Kreidieh, Dana El Masri, Marwan El Ghoch
World Journal of Diabetes.2019; 10(5): 311. CrossRef - Prognostic networks for unraveling the biological mechanisms of Sarcopenia
Ana Cernea, Juan Luis Fernández-Martínez, Enrique Juan de Andrés-Galiana, Zulima Fernández-Muñiz, Juan Carlos Bermejo-Millo, Laura González-Blanco, Juan José Solano, Pedro Abizanda, Ana Coto-Montes, Beatriz Caballero
Mechanisms of Ageing and Development.2019; 182: 111129. CrossRef - Malnutrition as a Complication of Bariatric Surgery – A Clear and Present Danger?
Jessica Lange, Alfred Königsrainer
Visceral Medicine.2019; 35(5): 305. CrossRef - 変形性膝関節症とサルコペニア肥満
Orthopedics & Traumatology.2018; 67(2): 350. CrossRef - Sarcopenic obesity
Stergios A. Polyzos, Andrew N. Margioris
Hormones.2018; 17(3): 321. CrossRef - Is sarcopenia and sarcopenic obesity associated with clinical and pathological outcomes in patients undergoing radical nephroureterectomy?
Neil J. Kocher, Syed Jafri, Samyuktha Balabhadra, Erik Lehman, Jacob Gardner, Kanupriya Vijay, Nabeel Sarwani, Jay D. Raman
Urologic Oncology: Seminars and Original Investigations.2018; 36(4): 156.e17. CrossRef - The association of low muscle mass with soluble receptor for advanced glycation end products (sRAGE): The Korean Sarcopenic Obesity Study (KSOS)
Tae Nyun Kim, Man Sik Park, Eun Joo Lee, Hye Soo Chung, Hye Jin Yoo, Hyun Joo Kang, Wook Song, Sei Hyun Baik, Kyung Mook Choi
Diabetes/Metabolism Research and Reviews.2018;[Epub] CrossRef - Lower-limb muscle strength according to bodyweight and muscle mass among middle age patients with type 2 diabetes without diabetic neuropathy
Fuminari Asada, Takuo Nomura, Mitsuo Tagami, Masashi Kubota, Makoto Ohashi, Makoto Nomura
Journal of Physical Therapy Science.2017; 29(7): 1181. CrossRef - Association between Sarcopenic Obesity and Metabolic Syndrome in Postmenopausal Women: A Cross-sectional Study Based on the Korean National Health and Nutritional Examination Surveys from 2008 to 2011
Sun-Young Kang, Gyeong Eun Lim, Yang Keun Kim, Hye Won Kim, Kayoung Lee, Tae-Jin Park, Jinseung Kim
Journal of Bone Metabolism.2017; 24(1): 9. CrossRef - Changes in Body Composition According to Age and Sex among Young Non-Diabetic Korean Adults: the Kangbuk Samsung Health Study
Seul-Ki Kim, Yu-Hyun Kwon, Jung Hwan Cho, Da Young Lee, Se Eun Park, Hyung-Geun Oh, Cheol-Young Park, Won-Young Lee, Ki-Won Oh, Sung-Woo Park, Eun-Jung Rhee
Endocrinology and Metabolism.2017; 32(4): 442. CrossRef - Health-related quality of life and activity limitation in an elderly Korean population with sarcopenia: The Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV-2, 3), 2008–2009
T.H. Kim, S.-H. Kim, J. Kim, H.-J. Hwang
European Geriatric Medicine.2017; 8(4): 360. CrossRef - Rheumatoid Cachexia, a Metabolic Rheumatoid Arthritis Disorder: Pathophysiological Mechanisms, Diagnostic Tools and Current Therapeutic Strategy
Imad Ghozlani
Endocrinology&Metabolism International Journal.2017;[Epub] CrossRef - Decreased muscle mass in Korean subjects with intracranial arterial stenosis: The Kangbuk Samsung Health Study
Ho-Jung Jung, Hwanseok Jung, Taeyoung Lee, Jongho Kim, Jongsin Park, Hacsoo Kim, Junghwan Cho, Won-Young Lee, Sung-Woo Park, Eun-Jung Rhee, Hyung-Geun Oh
Atherosclerosis.2017; 256: 89. CrossRef - Lower Jump Power Rather Than Muscle Mass Itself is Associated with Vertebral Fracture in Community-Dwelling Elderly Korean Women
Eun Young Lee, Su Jin Lee, Kyoung Min Kim, Da Hea Seo, Seung Won Lee, Han Sol Choi, Hyeon Chang Kim, Yoosik Youm, Chang Oh Kim, Yumie Rhee
Calcified Tissue International.2017; 100(6): 585. CrossRef - Effects of combination of change in visceral fat and thigh muscle mass on the development of type 2 diabetes
Seung Jin Han, Soo-Kyung Kim, Wilfred Y. Fujimoto, Steven E. Kahn, Donna L. Leonetti, Edward J. Boyko
Diabetes Research and Clinical Practice.2017; 134: 131. CrossRef - Comparisons of three different methods for defining sarcopenia: An aspect of cardiometabolic risk
Tae Nyun Kim, Man Sik Park, Eun Joo Lee, Hye Soo Chung, Hye Jin Yoo, Hyun Joo Kang, Wook Song, Sei Hyun Baik, Kyung Mook Choi
Scientific Reports.2017;[Epub] CrossRef - Association of metabolic syndrome and 25‐hydroxyvitamin D with cognitive impairment among elderly Koreans
Eun Young Lee, Su Jin Lee, Kyoung Min Kim, Young Mi Yun, Bo Mi Song, Jong Eun Kim, Hyeon Chang Kim, Yumie Rhee, Yoosik Youm, Chang Oh Kim
Geriatrics & Gerontology International.2017; 17(7): 1069. CrossRef - Sarcopenia and sarcopenic obesity in patients with complex abdominal wall hernias
John M. Rinaldi, Abby K. Geletzke, Brett E. Phillips, Jamie Miller, Thomas M. Dykes, David I. Soybel
The American Journal of Surgery.2016; 212(5): 903. CrossRef - Bariatric Surgery Outcomes in Sarcopenic Obesity
Diego Mastino, Maud Robert, Cecile Betry, Martine Laville, Christian Gouillat, Emmanuel Disse
Obesity Surgery.2016; 26(10): 2355. CrossRef - Sarcopenia in Orthopedic Surgery
Steven L. Bokshan, J. Mason DePasse, Alan H. Daniels
Orthopedics.2016;[Epub] CrossRef - Sarcopenia and Hearing Loss in Older Koreans: Findings from the Korea National Health and Nutrition Examination Survey (KNHANES) 2010
Jieun Lee, Kyungdo Han, Jae Jun Song, Gi Jung Im, Sung Won Chae, Stephen E Alway
PLOS ONE.2016; 11(3): e0150281. CrossRef - Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia
Kyoung Min Kim, Hak Chul Jang, Soo Lim
The Korean Journal of Internal Medicine.2016; 31(4): 643. CrossRef - Newly Developed Sarcopenia as a Prognostic Factor for Survival in Patients who Underwent Liver Transplantation
Ja Young Jeon, Hee-Jung Wang, So Young Ock, Weiguang Xu, Jung-Dong Lee, Jei Hee Lee, Hae Jin Kim, Dae Jung Kim, Kwan Woo Lee, Seung Jin Han, Erica Villa
PLOS ONE.2015; 10(11): e0143966. CrossRef - The effect of sarcopenic obesity on cardiovascular disease and all-cause mortality in older people
Janice L Atkins, S Goya Wannamethee
Reviews in Clinical Gerontology.2015; 25(2): 86. CrossRef - Low muscle mass is associated with metabolic syndrome only in nonobese young adults: the Korea National Health and Nutrition Examination Survey 2008-2010
Byung Chul Kim, Mee Kyoung Kim, Kyungdo Han, Sae-Young Lee, Seung-Hwan Lee, Seung-Hyun Ko, Hyuk-Sang Kwon, Anwar T. Merchant, Hyeon Woo Yim, Won-Chul Lee, Yong Gyu Park, Yong-Moon Park
Nutrition Research.2015; 35(12): 1070. CrossRef - Identifying subgroups of obesity using the product of triglycerides and glucose: the Korea National Health and Nutrition Examination Survey, 2008–2010
Seung‐Hwan Lee, Kyungdo Han, Hae Kyung Yang, Mee Kyoung Kim, Kun‐Ho Yoon, Hyuk‐Sang Kwon, Yong‐Moon Park
Clinical Endocrinology.2015; 82(2): 213. CrossRef - Effect of beta-hydroxy-beta-methylbutyrate supplementation on muscle loss in older adults: A systematic review and meta-analysis
Hongmei Wu, Yang Xia, Jin Jiang, Huanmin Du, Xiaoyan Guo, Xing Liu, Chunlei Li, Guowei Huang, Kaijun Niu
Archives of Gerontology and Geriatrics.2015; 61(2): 168. CrossRef - Muscle loss and obesity: the health implications of sarcopenia and sarcopenic obesity
S. Goya Wannamethee, Janice L. Atkins
Proceedings of the Nutrition Society.2015; 74(4): 405. CrossRef - Subclinical vascular inflammation in subjects with normal weight obesity and its association with body Fat: an 18 F-FDG-PET/CT study
Shinae Kang, Chanhee Kyung, Jong Suk Park, Sohee Kim, Seung-Pyo Lee, Min Kyung Kim, Hye Kyung Kim, Kyung Rae Kim, Tae Joo Jeon, Chul Woo Ahn
Cardiovascular Diabetology.2014;[Epub] CrossRef - Using mobile phones in healthcare management for the elderly
Hun-Sung Kim, Kye-Hwa Lee, Hyunah Kim, Ju Han Kim
Maturitas.2014; 79(4): 381. CrossRef - Sarcopenia as a Determinant of Blood Pressure in Older Koreans: Findings from the Korea National Health and Nutrition Examination Surveys (KNHANES) 2008–2010
Kyungdo Han, Yu-Mi Park, Hyuk-Sang Kwon, Seung-Hyun Ko, Seung-Hwan Lee, Hyeon Woo Yim, Won-Chul Lee, Yong Gyu Park, Mee Kyoung Kim, Yong-Moon Park, Yan Li
PLoS ONE.2014; 9(1): e86902. CrossRef - An Overview of the Identification and Management of the Metabolic Syndrome in Chiropractic Practice
David R. Seaman, Adam D. Palombo
Journal of Chiropractic Medicine.2014; 13(3): 210. CrossRef - Sarcopenia and Neurosurgery
Seung Won Park
Journal of Korean Neurosurgical Society.2014; 56(2): 79. CrossRef - Growing healthy muscles to optimise metabolic health into adult life
S. A. Bayol, C. R. Bruce, G. D. Wadley
Journal of Developmental Origins of Health and Disease.2014; 5(6): 420. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef - Variation in Serum Creatinine Level Is Correlated to Risk of Type 2 Diabetes
Jun Sung Moon, Ji Eun Lee, Ji Sung Yoon
Endocrinology and Metabolism.2013; 28(3): 207. CrossRef
- Influence of Sugar-Sweetened Beverages Intake on Sarcopenic Obesity, Visceral Obesity, and Sarcopenia in Lebanese Patients with MASLD: A Case-Control Study

- A Case of Multiple Osteoporotic Compression Fractures in Young Man with Budd-Chiari Syndrome.
- Sun Hwa Kim, Tae Un Yang, Byeong Kwang Choi, Hye Jin Yoo, Ji A Seo, Kyung Mook Choi, Nan Hee Kim, Sin Gon Kim, Sei Hyun Baik, Dong Seop Choi, Hae Yoon Choi
- Endocrinol Metab. 2012;27(4):334-339. Published online December 20, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.4.334
- 2,015 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Osteoporosis in young men is extremely rare. In this report, we demonstrate a rare case of multiple vertebral fractures discovered in a young man with Budd-Chiari syndrome without prior history of trauma. A 29-year-old man was diagnosed as Budd-Chiari syndrome 12 years ago and underwent a mesocaval shunt to relieve the hepatic vein obstruction and was on warfarin therapy. He suffered from low back pain and it was not relieved by analgesics. A T-L spine X-ray revealed multiple compression fractures and the z-score at lumbar spine was -3.7 which is below the expected range for that age. The patient was treated with calcium, vitamin D and bisphosphonate, and showed clinical improvement. This case highlights the importance of the investigation for secondary osteoporosis in young adults with an underlying disease that alters bone metabolism.

- Thyroid Dysfunction of North Korean Women Living in South Korea, Focusing on Subclinical Hypothyroidism.
- Joo Hyung Kim, Sol Ah Park, Nam Hoon Kim, Jae Hee Ahn, Yoon Jung Kim, Myongjin Cho, Yoon Jung Lee, Hye Jin Yoo, Hee Young Kim, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Sin Gon Kim
- Endocrinol Metab. 2012;27(3):200-207. Published online September 19, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.3.200
- 3,513 View
- 27 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Thyroid function depends on ethnic and environmental factors. North Korean refugees have the same genetic background as South Koreans, but they have been exposed to different environments. This study examines the prevalence and pattern of thyroid disorders in North Korean women living in South Korea, focusing on subclinical hypothyroidism (SCH). METHODS: The intended sample was a total of 327 North Korean women residing in Seoul. Health questionnaires and medical examinations, including serum thyrotropin (thyroid stimulating hormone, TSH), free thyroxine, and thyroid autoantibodies, were conducted. RESULTS: The prevalence of SCH was 9.4%. In logistic regression analysis, smoking, menopause, length of stay in South Korea, body mass index, history of thyroid disease, and metabolic syndrome were not associated with the risk of SCH. Whereas, the positivity of autoantibodies were associated with a high risk for SCH (odds ratio [OR], 4.840; 95% confidence interval [CI], 1.80-13.017; P = 0.002), and age was associated with a low risk for SCH (OR, 0.94; 95% CI, 0.888-0.994; P = 0.031). The serum TSH levels also decreased with increasing age, and in particular, there was significant difference between 30-39 years, and over 60 years (2.33 +/- 1.51 microIU/mL vs. 1.54 +/- 0.73 microIU/mL, P = 0.028). CONCLUSION: In North Korean women, the positivity of autoantibodies was associated with a high risk for SCH. But interestingly, a younger age was associated with a high risk for SCH. Considering that they suffered from severe famine at the period of growth, and this led to malnutrition, their thyroid dysfunction might be associated with the peculiar environment that they experienced. -
Citations
Citations to this article as recorded by- Systematic review of evidence on public health in the Democratic People’s Republic of Korea
John J Park, Ah-Young Lim, Hyung-Soon Ahn, Andrew I Kim, Soyoung Choi, David HW Oh, Owen Lee-Park, Sharon Y Kim, Sun Jae Jung, Jesse B Bump, Rifat Atun, Hee Young Shin, Kee B Park
BMJ Global Health.2019; 4(2): e001133. CrossRef - Environmental Factors and Thyroid Dysfunction
Hyun-Kyung Chung
Endocrinology and Metabolism.2012; 27(3): 191. CrossRef
- Systematic review of evidence on public health in the Democratic People’s Republic of Korea


 KES
KES

 First
First Prev
Prev



